Because I work with cancer patients and because many are completely shocked by the fact that I recommend eating meat and dairy despite the existence on Earth of the book entitled “The China Study”, in this article and in the following one I will present the aspects that invalidate the main assumptions in this book called „study“.
First of all, I would like to point out that there is no diet to cure cancer.
No diet, no dietary supplement and no plant remedy cures cancer. NONE.
Cancer is a piece of our own body that managed to become so adaptable, aggressive, and capable of camouflage like a chameleon – it knows all our defensive secrets inside out, it uses all our defense mechanisms against its own body.
As a patient – the belief that the natural healer can cure your cancer with antioxidants, mushrooms, teas, sins forgiveness, Karma cleanses, or ginseng powdered magic pills sprinkled with star dust can be understood based on the confusion and on the feeling that you just lost of control over your own life, feelings commonly associated with a cancer diagnosis.
But to promote that you – the “Carpathian quack” – can naturally cure cancer on your own equals either an incapacity to understand what you’re fighting with, or an equally callousness, both sold to desperate patients for hard earned money and end of life hopes.
A true pseudo-medical industry has flourished on the basis of the confusion and despair of oncological patients.
However, because of its high adaptability and aggressivity, cancer treatment requires one of the most multidisciplinary approaches possible. And, even so, the war with cancer is not won by default because the malignant cells are extraordinarily unpredictable.
By oncology nutrition we do not cure cancer, we only support the effectiveness of oncology treatment, counteracting side effects as much as possible and only when this is possible without influencing treatment efficacy.
Oncology nutrition means moderate consumption of high quality food of both vegetable and animal origin, consumption carefully adapted to the body weight, body composition, appetite impairment, any other non-oncological associated pathologies the individual patient might have, and to the actual oncology treatment stage and its side effects.
Extremes such as “you can eat everything” are just as damaging as the extremes “don’t drink milk (1), don’t eat meat (2), or take a waggon of antioxidants” (3).
Firstly, I would like to underline that oncology nutrition is just highly personalised clinical nutrition simply because we cannot starve cancer. There are many mechanisms behind this avoidance extreme dietary recommendation, but the main ones are the following:
- malignant cells are a true “black hole” for glucose because they have much more glucose transporters than any normal cell could ever have (4) – and it simply doesn’t matter if this glucose is obtained by the tumour from consuming glucose from rice, corn, potatoes, pasta, bread, sweets, fruits, honey; or from the glucose produced inside the body from amino acids or glycerol when glucose intake is restricted
- malignant cells can use antioxidants to survive despite treatment administration, which is exactly why the antioxidant co-administration can decrease the efficacy of oncological treatment (5).
But the fact that we recommend moderate consumption of meat, fish, eggs and dairy products during oncological treatment – besides the moderate consumption of fruits, vegetables and whole grains – does not mean that we recommend the consumption of roasted eggs, donuts, bacon, fried cheese or soda drinks.
Even Campbell himself said that such simplistic thinking is idiotic:
“Everything in food works together to create health. The more we think that a single chemical characterises a whole food, the more we stray into idiocy”.
(“The China Study”, page 106)
Secondly, I would also like to underline that:
- Epidemiology studies results are correlations, not causality evidence.
- And correlations are invalid if the issue at hand can be generated by other bias factors that have not been taken into account by the researches that did that particular study.
So, despite the popularity, the book entitled “The China Study” at most raises hypotheses, it does not bring any causal evidence about the link between foods and cancer.
The main findings associated with a cancer risk presented in this book – findings listed on the Cornell University website – are the following:
- Plasma cholesterol in the 90-170 milligrams per deciliter range is positively associated with most cancer mortality rates. Plasma cholesterol is positively associated with animal protein intake and inversely associated with plant protein intake.
- Breast cancer is associated with dietary fat (which is associated with animal protein intake) and inversely with age at menarche (women who reach puberty at younger ages have a greater risk of breast cancer).
- For those at risk for liver cancer (for example, because of chronic infection with hepatitis B virus) increasing intakes of animal-based foods and/or increasing concentrations of plasma cholesterol are associated with a higher disease risk.
- Colorectal cancers are consistently inversely associated with intakes of 14 different dietary fiber fractions (although only one is statistically significant). Stomach cancer is inversely associated with green vegetable intake and plasma concentrations of beta-carotene and vitamin C obtained only from plant-based foods.
- Western-type diseases, in the aggregate, are highly significantly correlated with increasing concentrations of plasma cholesterol, which are associated in turn with increasing intakes of animal-based foods.
Before we discuss about the fact that the increased risk of cancer associated by Campbell to animal-based foods can be at most be interfered indirectly through hypercholesterolemia potentially associated with the fat contained by such foods as no conclusive association “animal protein” is made.
Thus, it would be logical to ask ourselves some questions:
– What is the essential difference between “animal protein” and “vegetable protein”?
– Why would vegetable protein intake be protective while animal protein intake harmful?
– And doesn’t categorising all animal-based foods’ as “bad” based on the inferred impact of a single isolated substance increases the risk of idiocy, according to Campbell’s own words?
Leaving aside the fact that there is a multitude of animal proteins and a multitude of vegetable proteins, their simplistic definition of as “animal protein” or “vegetable protein” can only be made on the basis of their essential amino acid content.
Humans do not feed with proteins, but with foods that are digested up to amino acids to be absorbed through the intestinal wall.
The only difference between “animal protein” and “vegetal protein” is that the vegetal protein does not contain all the essential amino acids.
– So, if the “animal protein” is somehow carcinogenic because it has all the essential amino acids, why would the combination of vegetal protein recommended to the vegans to ensure the proper essential amino acid intake be as carcinogenic as the intake of meat?
Because, basically, if we consider not only the generic concept of “protein intake”, but also the fact that the eaten food must be digested up to amino acids in order to pass through the intestinal wall, all we have after protein digestion are:
- all essential amino acids – after digesting proteins of animal origin
- only a part of them – after digesting proteins of plant origin
- all essential amino acids – after digesting a mixed meal composed of plant proteins with complementary amino acid intake
But nowhere in this book called “study” is it demonstrated that animal protein intake feeds cancer, increases cancer risk or that it decreases in any way the survival of cancer patients. Paradoxically, the mentality behind the nutritional recommendations in “The China study” is completely unrelated to any protein, being inferred from fats not from proteins:
Hypercholesterolaemia increases the risk of cancer and mortality.
Foods of animal origin contain cholesterol, so they raise cholesterol.
Foods of plant origin do not contain cholesterol, so they lower cholesterol.
Inference 1: Foods of plant origin decrease cancer risk.
Inference 2: Foods of animal origin increase cancer risk.
Foods of plant origin contain animal protein.
Conclusion: Foods of animal origin increase cancer risk.
But there are a lot of BUTs.
The database used by Campbell to draw these conclusions did not belong to him, the “evidence” behind his book being published in 1990 by Zhongguo by Shan Shi, Sheng Huo Fang Shi He Si Wang and Junshi Chen in Diet, Life-Style, and Mortality in China: A Study of the Characteristics of 65 Chinese Counties.
And, despite the opinion of many natural healing gurus, this database is not about the fact that due to the traditional Chinese diet China’s population has a lowed risk of cancer or a lower cancer related mortality. Not even close.
Unfortunately, China occupies one of the leading positions in cancer statistics, and the rural residents of China have a much higher cancer incidence and mortality than those living in the cities (6).
The study on which Campbell’s book is based is an epidemiological study based on a questionnaire in which respondents were asked to check boxes of pre-filled tables with various foods and written fixed quantities – the foods they had consumed in the last 3 days, followed by blood and urine analysis. Then the statical results obtained from this questionnaire were correlated with the cancer related mortality calculated for that particular area 10 years prior to the study.
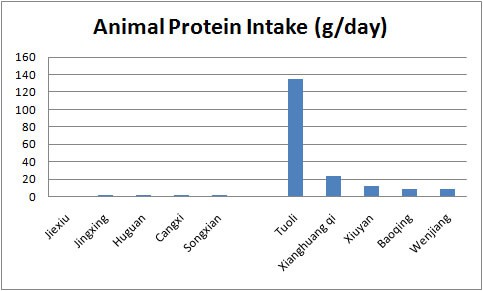
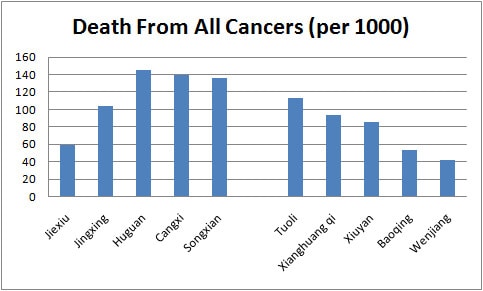
Junshi Chen and his colleagues chose to do this epidemiological study because the rural Chinese people of the 1980s used to live their entire life in the same region without altering their lifestyle and diet, and because of the vast geographical areas there are very large differences in lifestyle and nutrition from one Chinese region to another: the inhabitants of some areas being traditionally almost vegan, while the inhabitants of other regions traditionally consuming ± 1 kg of dairy products per day simply because they were shepherds.
But these researchers quoted by Campbell found only a mild correlation with no statistical significance between animal protein intake and cancer (+ 3% overall risk for mortality due to any type of cancer) and a slightly higher correlation for vegetable protein intake and cancer (+ 12% overall risk for mortality due to any type of cancer):
- Risk of cancer mortality correlated to the animal protein intake
Lymphoma: -18
Bladder cancer: -9
Colorectal cancer: -8
Leukemia: -5
Nasopharyngeal cancer: -4
Cervical cancer: -4
Liver cancer: -3
Cancer of esophagus: +2
Breast cancer: +12
- Risk of cancer related mortality correlated with vegetable protein intake
Lymphoma: -4
Bladder cancer: -3
Colorectal cancer: +19
Leukemia: +15
Nasopharyngeal cancer: -40*
Cervical cancer: +12
Liver cancer: +12
Cancer of esophagus: +18
Breast cancer: +1
But correlations without * are not statistically valid and the obtained values increase in statistical significance when they have two or three asterixes (p<0.05 = * statistically significant; p<0.001 = ** more statistically significant; p<0.0001 = *** very statistically significant).
Also, in order to be able to raise a risk factor hypothesis, we must take into account any other confounding factors that can also be correlated with the particular risk we are trying to evaluate.
For example, for breast cancer – besides non-statistical correlations generated by the consumption of proteins, be it animal or vegetable – there are other correlations, some significant, some not:
- Hyperglycemia: +36**
- Wine consumption: +33*
- Alcohol consumption: +31*
- Fruit intake: +25
- Workplace in industry (as opposed to agriculture): +24
- Sweets and flour products intake: +20
- Beer intake: +19
- Legumes intake: +17
I underline again that these are “correlations” – either positive = risk factor, either negative = protective factor; either statistically valid if they have *, either with no statistical significance if they do not have *. Correlations are not causal evidence.
And Junshi Chen and his collaborators have not found any statistically significant correlations between animal protein intake and cancer risk or with cancer related mortality.
For instance, their respondents from one of the areas with the highest animal-protein intake (Tuoli) had lower rates of cancer related mortality risks than those from areas with almost zero animal protein intake (Huguan).
So 1: Ignore the fact that Campbell nutritional recommendations are contradicted by the very researchers he quoted as proof.
These were other researchers.
Despite the fact that a researcher like Campbell quoted their correlations as arguments in support of his conclusions, these other researchers might have been wrong.
It seems incredible, however, that he used his 1983 study to prove that the “animal protein” feeds malignant cells by “activating” cancer, because – unlike popular opinion believed by many – the results of his own study was not that 20% casein-fed mice developed tumours, and that mice fed with 5% lived happily ever after, learning their grandchildren about the benefits of veganism (7).
His own study protocol was as follows:
- two groups of mice were fed for 2 weeks with either 5% casein or 20% casein while administered aflatoxin.
- then each group was divided into two, and each of the two new subgroups was fed either with 5% casein or with 20% casein for another 12 weeks.
And please keep in mind that aflatoxin was the carcinogen in this whole story, not casein (8).
You can see the results in Tables 1 and 2 of the picture below (with the mention that you can read the entire English study by clicking on the link to the study quoted under No. 7).
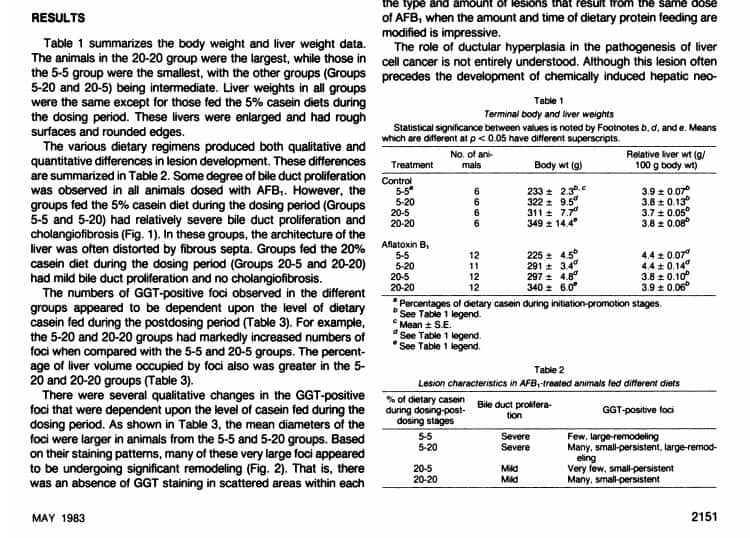
So, Campbell’s own results were the following:
- The group fed with 5% casein during the administration of the aflatoxin carcinogen developed severe hepatic lesions (hepatomegaly, cholangiofibrosis, and bile duct proliferation)
- The group fed with 20% casein on the duration of the aflatoxin carcinogen developed only rare moderate hepatic lesions (no colangiofibrosis or bile duct proliferation)
And this was no surprise for him, Campbell demonstrating in another of his earlier studies that aflatoxin is far more carcinogenic in case of insufficient protein intake (9).
– And I would sometimes like to ask those who advise cancer patients to become vegans: Do you understand that you basically advise these poor sick people to adhere to a diet that increases the toxicity of carcinogens?
Nowhere in this study, Campbell has shown that mice fed with 20% casein have cancer or those with 5% did not. What his study demonstrates is that hepatic lesions developed by 5% casein fed mice are different and more severe than those developed by mice fed with 20% casein.
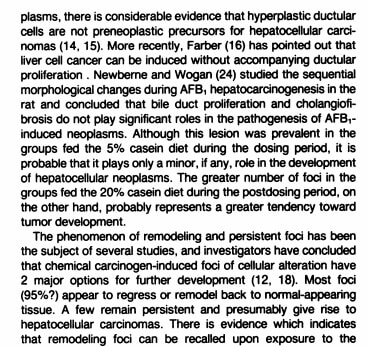
Campbell points out that:
- biliary duct hyperplasia and cholangiofibrosis are not pre-neoplastic lesions;
- the lesions developed in 20% casein-fed mice “probably have a higher tendency towards tumour growth”;
- although in the next paragraph he writes that most of these lesions regress, transforming back into normal tissue, and that only a few of them persist, probably generating tumours.
None of the mice in the Campbell’s study died of even developed cancer, regardless of their diet.
– How does that sound as a scientific evidence that animal protein intake is carcinogenic?
As I write above, using such a study to support the casein harm looks unbelievable. And it looked unbelievable also to the Indian researchers Mathur and Nayak, who tried in 1989 to recreate Campbell’s results using the same aflatoxin protocol while feeding 5% and 20% casein monkeys, not mice (10).
The results of this study demonstrated once again what Campbell had actually obtained = a higher casein intake provides hepatic protection and increased survival even in the presence of aflatoxin exposure:
- most monkeys fed with 5% casein died before 70 weeks before they started developing liver tumors
- monkeys fed with 5% casein that survived for more than 90 weeks developed preneoplastic liver lesions
- monkeys fed with 20% casein did not develop any preneoplastic hepatic injury (the exact words of the researchers are: “The animals in the high protein group surviving even beyond 90 weeks do not show any preneoplastic / neoplastic lesions”.)
Thus, unlike Campbell – whose study showed the same protective effect of casein, but who chose ignore his own study results in order to present his his own personal view – Mathur and Nayak concluded that the protein-caloric malnutrition combined with the intake of aflatoxin contaminated foods explain the increased incidence of liver cancer in areas where these two factors co-exist.
I will explain more about casein and aflatoxin in particular and about the importance of dairy intake during oncological treatment generally in the part II of this article.
So 2: Please ignore the fact that a higher intake of casein protects the liver and increases survival even when exposed to a carcinogen as strong as aflatoxin.
Furthermore, the correlation between hypercholesterolemia and an increased risk of cancer is very far-fetched (11).
At nowadays’ hypercholesterolemia incidence, we could perorate bizarre correlations like:
- The school is carcinogenic because it keeps children nailed down in school benches for long, long hours – sedentariness increases cholesterol, so attending school increases the risk of cancer.
- Pokemon reduces the risk of cancer because the egg has to be walked 10 km – so when you play Pokemon you are no longer sedentary, thus playing Pokemon lowers your cholesterol, thus playing Pokemon reduces the risk of cancer.
Jokes aside, even if we accept that hypercholesterolemia would be so carcinogenic as Campbell paints it to be – despite the fact that current scientific literature does not support this hypothesis – to conclude that foods of animal origin increase the cancer risk because their intake might generate hypercholesterolemia is scientifically incredible.
The hypothesis that “the intake of foods of animal origin is the cause of hypercholesterolemia:
– puts under the same label:
- Fried schnitzels and steaks of lean meat baked in the oven – simply calling them both “meat” (12);
- Fried oil with extra virgin olive oil – simply calling them both “vegetable oil” (13);
- Fried potatoes or chips with baked or boiled potatoes – simply calling “potatoes” (14).
– does not take into account that we can make cholesterol inside the body from carbohydrates consumed in excess (15).
Of course, we can educate people with the Dr. Google, but researchers should not allow even researchers like Campbell to ignore any other lifestyle factors that can lead to hypercholesterolemia or any other pathologies or medications that can potentially increase both cholesterol and the cancer risk.
For example, it seems to be common sense to believe that increased fiber intake protects against colon cancer (16).
But – leaving common sense aside because it’s no longer that common these days – many of the respondents of the Junshi Chen study quoted by Campbell were infected with schistosomia – a risk factor for both hypercholesterolemia and colon and bladder cancer (17, 18).
Thus – because this parasite can cause both hypercholesterolemia and cancer – it would be logical to exclude schistosomia infected respondents from a population you study in order to draw a valid scientific conclusion about risk factors that can cause cancer.
But Campbell did not exclude them, hiding under the carpet also the fact that schistosomia increases the hypercholesterolemia and cancer risk.
So 3: If you agree to consider animal protein carcinogenic because animals have cholesterol and plants don’t, please ignore any other possible causes of hypercholesterolemia.
In marketing, there is a principle that sells well and can even make blackened bananas go viral:
Keep
It
Simply
Stupid
Congruently, Campbell keeps it as simple and as stupidly possible:
„Hypercholesterolemia increases the cancer risk.
Foods of animal origin contain cholesterol, thus their intake increase cholesterol, thus their intake increases cancer risk.
Foods of plant origin don not contain cholesterol, thus their intake does not increase cholesterol, thus their intake decreases cancer risk.
– So what if the researchers you are quoting concluded that plant protein intake is correlated with a higher cancer mortality risk?
– So what if you name casein a carcinogenic despite your own studies results?
– So what if hypercholesterolemia is not considered carcinogenic?
– So what if the patients whose cancer you claim to be caused by animal protein intake also had schistosomia?
Despite your very own scientific evidence, you are Campbell and you decided to follow marketing guidelines and to keep things simply stupid: „Consumption of any quantity of animal food increases the cancer risk and mortality through cancer“.
– Why should anyone use their logic when a biochemistry professor makes clinical recommendations based on extrapolations contradicted by the quoted epidemiological data and by his very own results?
Quoted studies





